Why do symptoms sometimes appear only in adulthood?
1 Embryology and the Growth Race
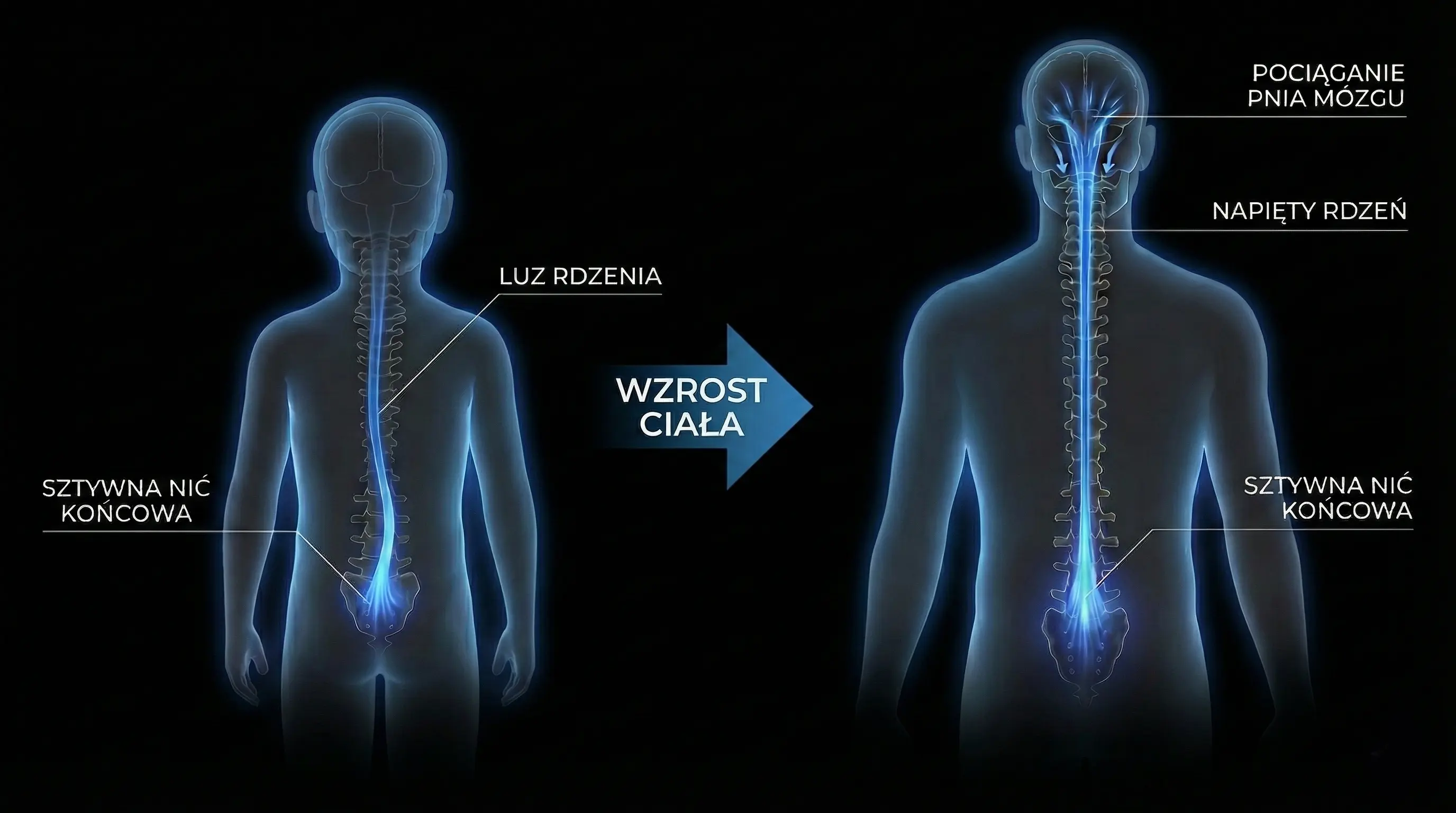
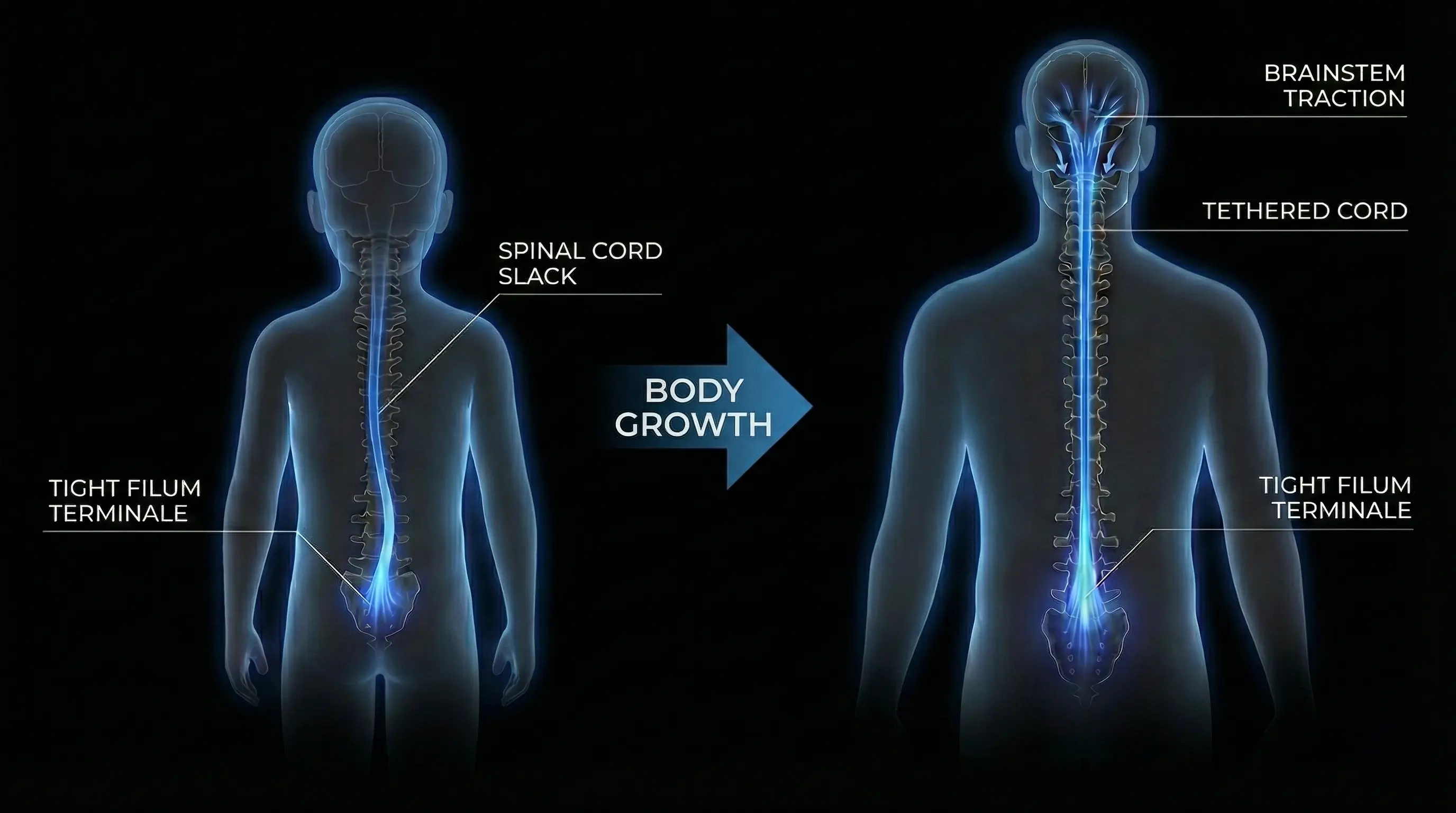
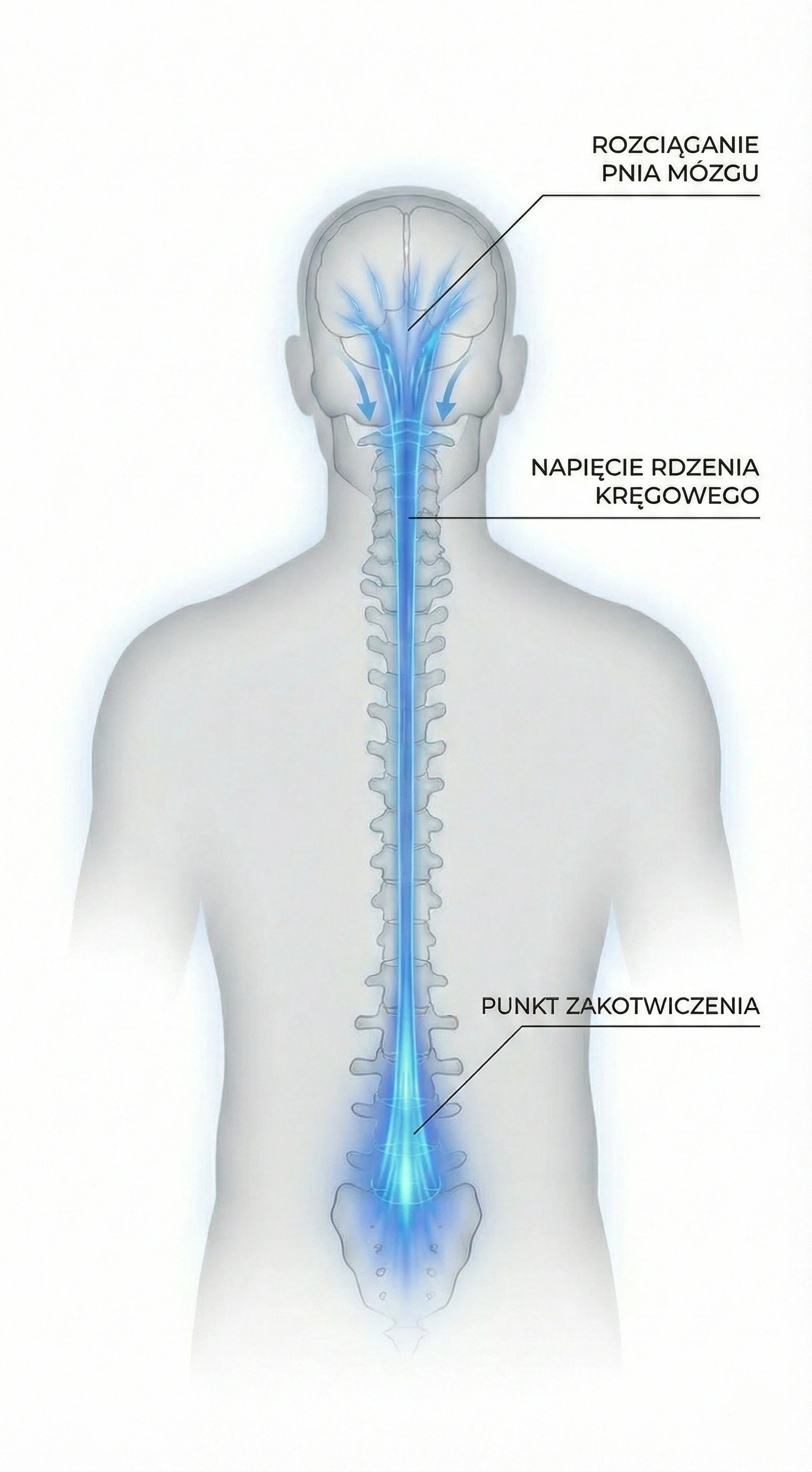
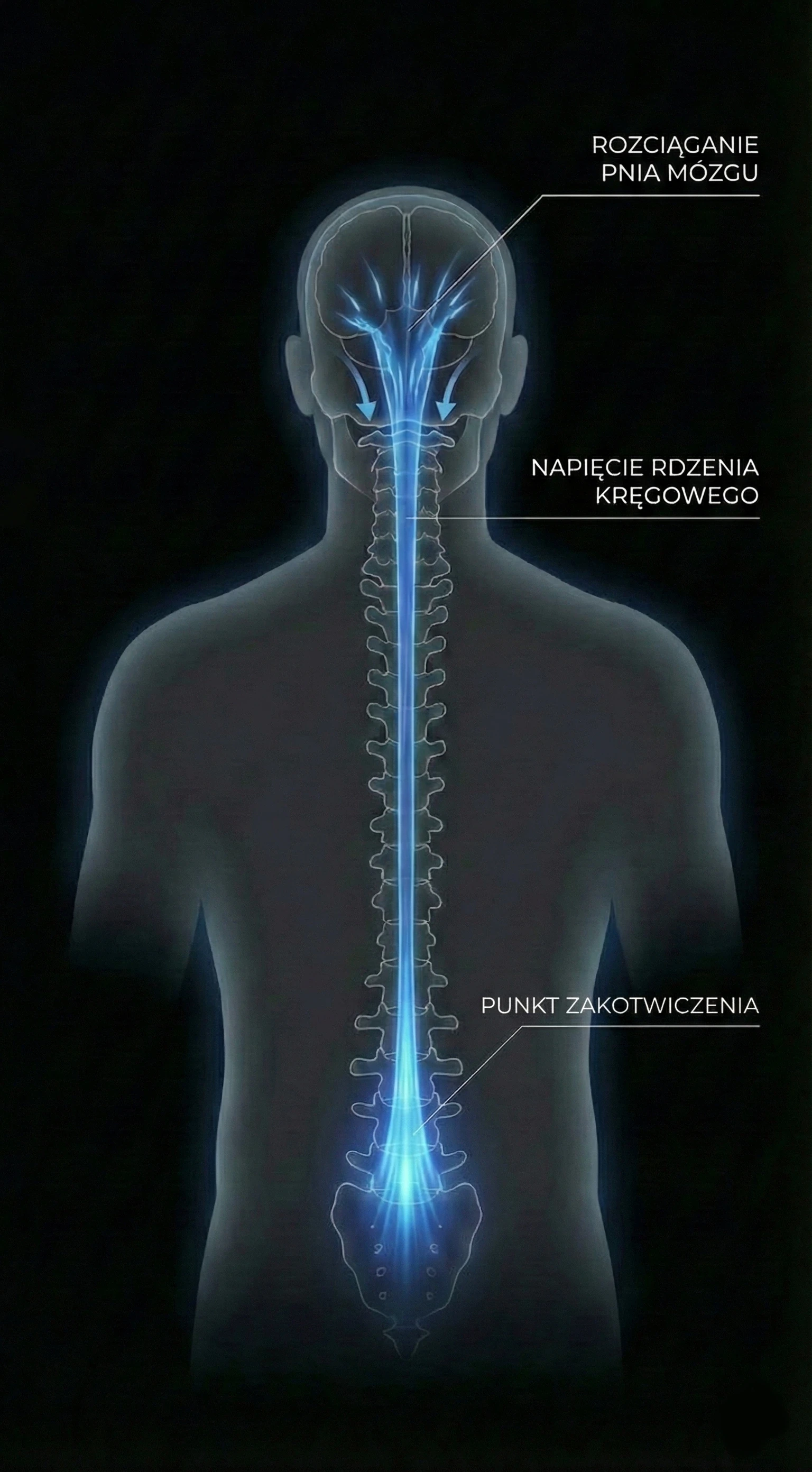
This phenomenon is called Ascensus Medullae. In fetal life, the spine (bones) grows much faster than the spinal cord (nerves). In a healthy person, the cord "pulls up" the spinal canal.
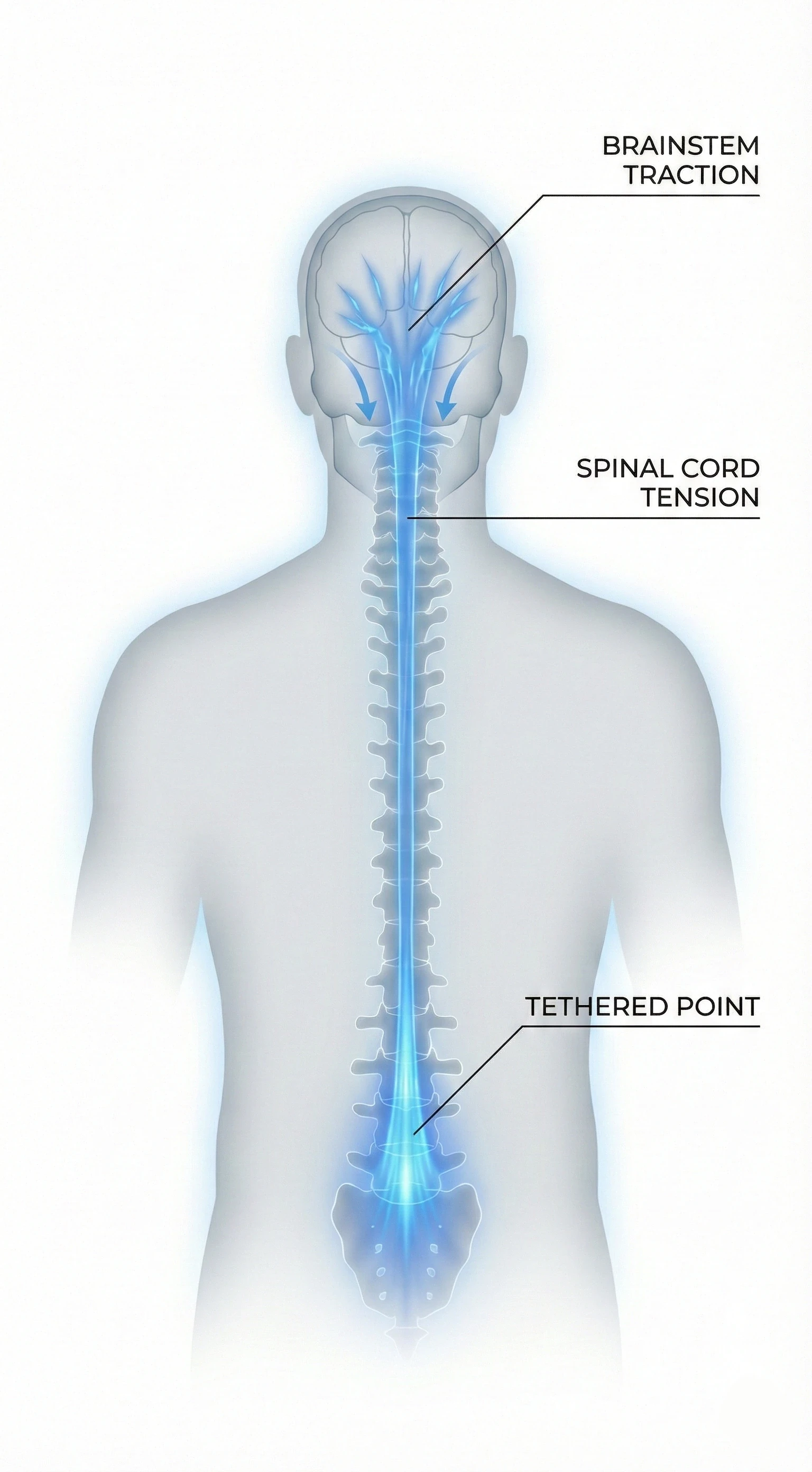
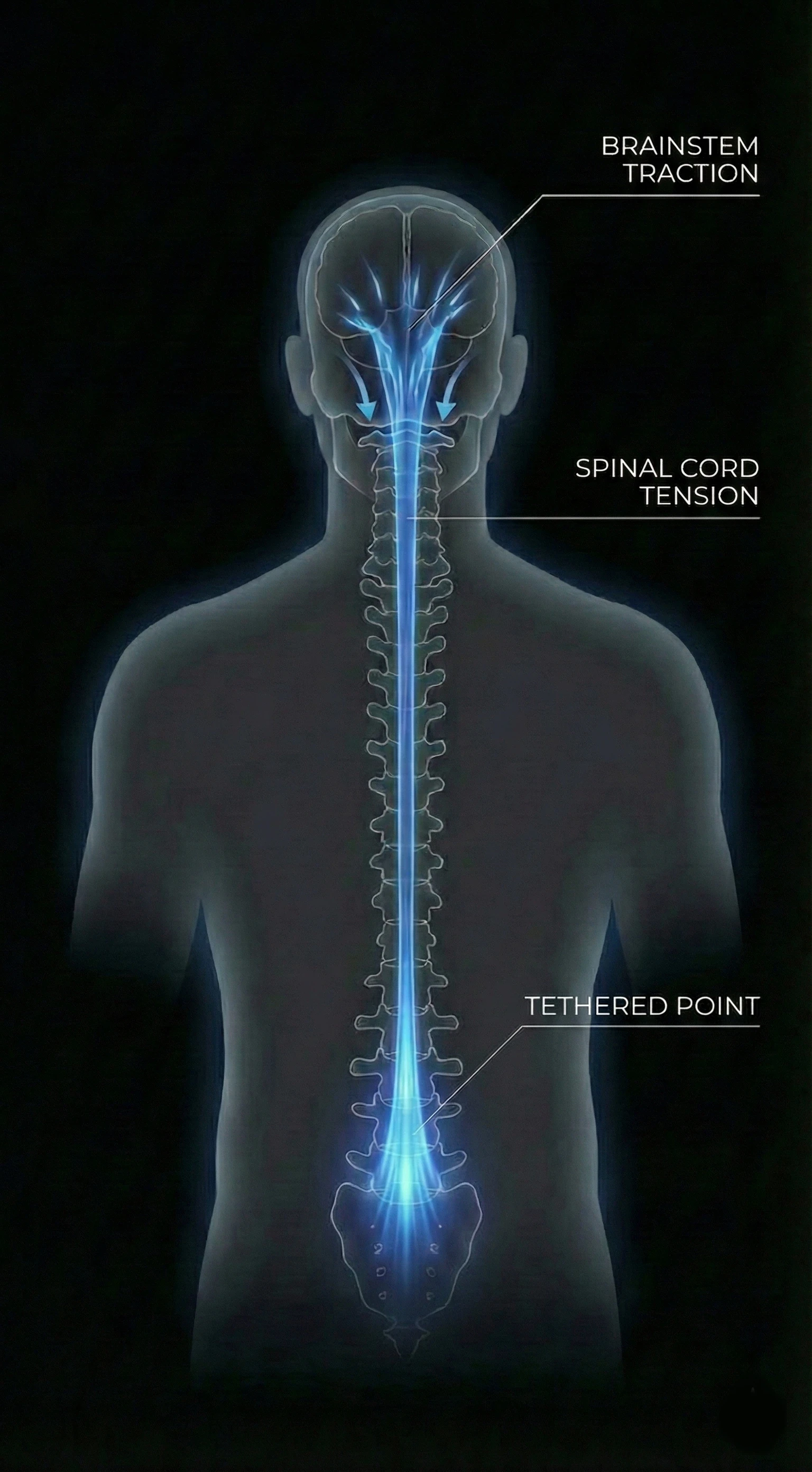
The process of spinal cord ascent (Ascensus Medullae) failed in childhood. The cord remained 'tethered'. In adulthood, symptoms erupt because tissues lose elasticity (collagen stiffening) and the spine accumulates years of micro-trauma. It is not bone growth that is the problem now, but the loss of elasticity reserve.
2 2. The "Tipping Point" Theory
"Why didn't I have symptoms as a child?"
The body has amazing adaptive capabilities, but only up to a point. With age, three things happen that take away the "slack reserve":
- Loss of Elasticity (Fibrosis): Tissues, including nerves and the filum terminale, stiffen and lose their ability to stretch.
- Accumulation of Microtrauma: Thousands of bends, falls, and movements over the years add up, weakening the cord's tolerance.
- Spinal Changes: Disc herniations or degeneration further compress or stretch the already tensioned cord.
At some point (often between ages 20 and 40), the sum of these factors crosses the "Tipping Point". The nervous system says "enough" and a cascade of symptoms appears.
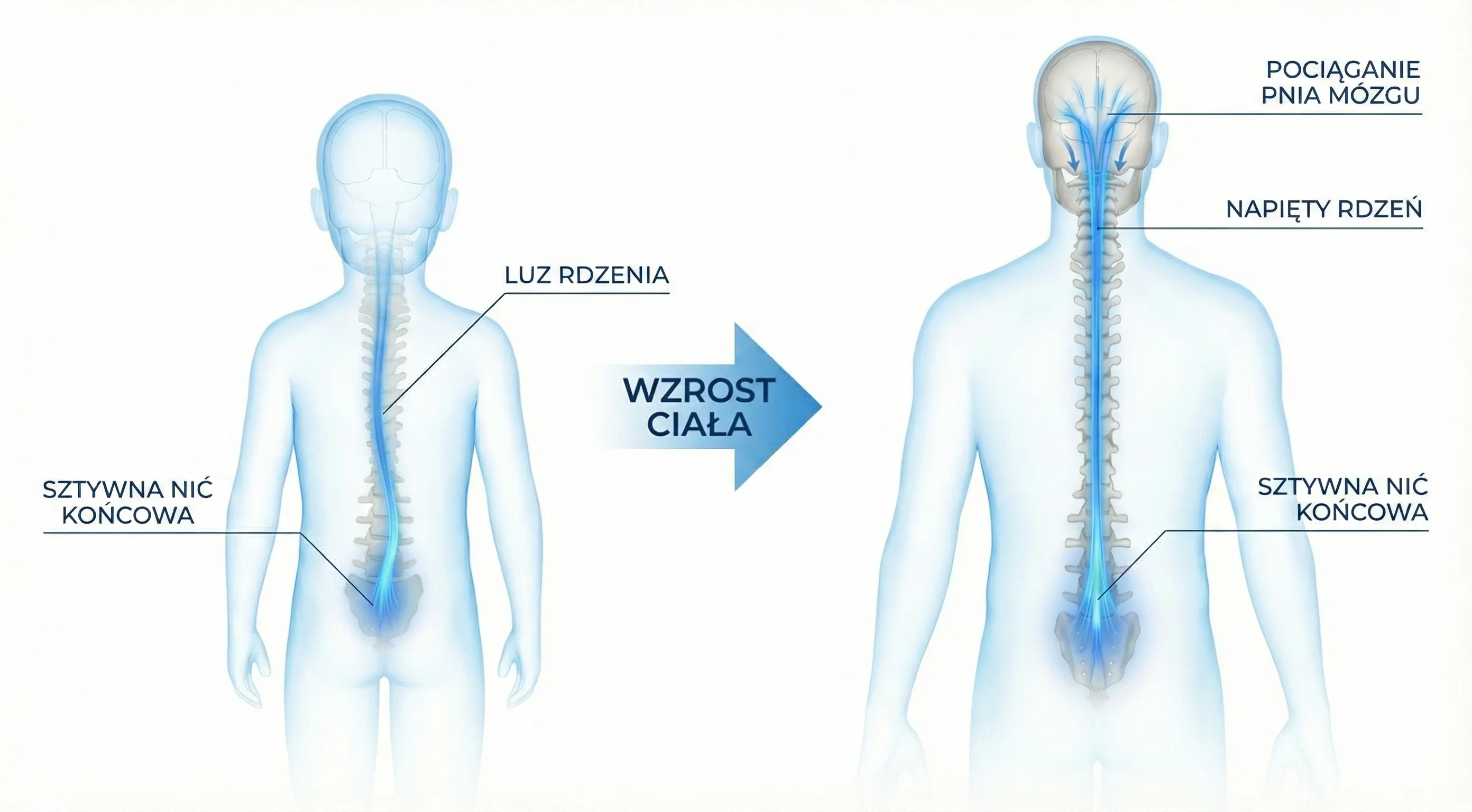
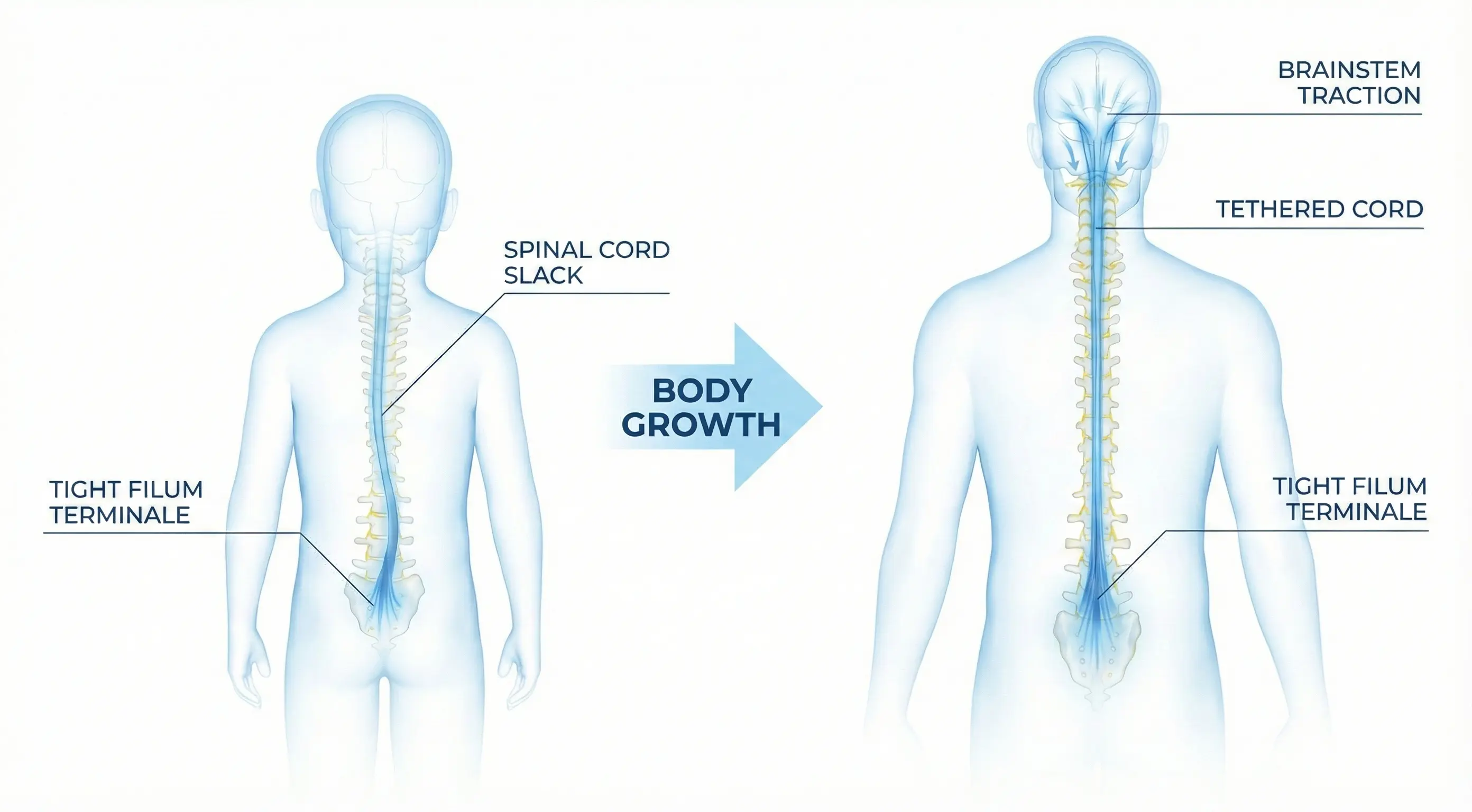
Visualization of Ascensus Medullae / Tipping Point